
Alcohol. Think Again Resources
The Alcohol. Think Again campaign is aimed at reducing risky alcohol use by changing the way people think about alcohol.
Access a range of evidence-based tools, guidelines, and training materials to support the mental health, alcohol, and other drug sector. These resources are designed to assist clinicians and service providers in delivering high-quality care across Western Australia.
Information on how and where workers in the community services sector are able to safely apply, remove and dispose of their PPE.
When deciding which Personal Protective Equipment (PPE) is required for different situations, it is important to follow your organisations policies and also refer to the decision tree in the WA Department of Health’s Advice for use of PPE for workers in community settings.
There are standard steps that must be followed when putting on and removing PPE. These apply across all sectors and the Department of Health provides this comprehensive guide on the process.
However, in the community services sector there are a number of variables that will impact how, and where workers will be able to safely apply, remove and dispose of their PPE.
The videos below demonstrate the considerations that the community services sector workforce needs to take into account when using PPE in different work settings.
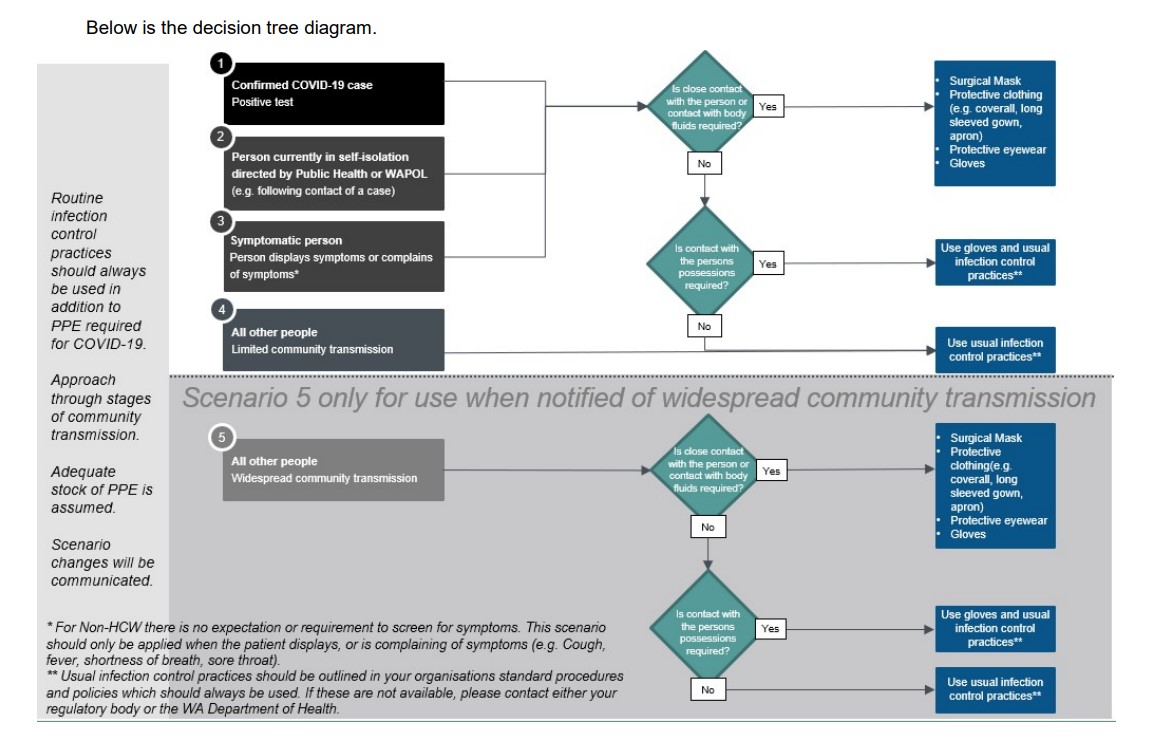
Department of Health Decision Tree (current as of 27 August 2020)
PPE considerations when transporting clients, and if organisational policies and the Department of Health decision tree stipulate that only a mask and gloves are required:
PPE considerations when working in a community sector setting such as a drop-in centre, refuge, or accommodation lodging, and if organisational policies and the Department of Health decision tree stipulate that full PPE (mask, gown, eyewear and gloves) is required:
PPE considerations when conducting a home visit, and if organisational policies and the Department of Health decision tree stipulate that full PPE (mask, gown, eyewear and gloves) is required:
The Mental Health Commission thanks Ruah Community Services and St Patrick’s Community Support Centre for their assistance in producing these videos.
See below for a range of resources to support the workforce to reduce alcohol and other drug related harms.
Opioids are depressant drugs that slow down brain activity. Most of the time opioids are used to manage pain but some people use them to experience feelings of euphoria and relaxation. Examples of opioids include oxycodone, fentanyl, methadone, heroin and nitazenes.
An opioid overdose occurs when the opioids disrupt breathing, causing it to either slow and/or stop. In 2023, opioids accounted for the largest proportion of drug overdose deaths in Western Australia.1 Pharmaceutical opioids were involved in most of these deaths.1
Naloxone is a medication that temporarily reverses the effects of an opioid overdose by restoring the person’s breathing. It starts to work within 2-5 minutes and lasts for up to 90 minutes. Naloxone is safe and easy to use and has no other effects other than to reverse the effect of opioids.
Naloxone is available free from organisations participating in the Commonwealth Take-Home Naloxone (THN) Program. It can also be prescribed by a doctor and purchased from a non-participating pharmacy.
Find registered sites near me
The Mental Health Commission (Commission) offers free online training for anyone who might experience or witness an opioid overdose. The training describes how to recognise an opioid overdose and how to respond using naloxone.
Access ‘Opioid Overdose and the Use of Naloxone’ training
Please note this training does not authorise a person to supply naloxone. Please contact naloxone@mhc.wa.gov.au for more information.
The Commission runs the WA Naloxone Program and oversees implementation of the Commonwealth THN Program in Western Australia. The WA Naloxone Program supports organisations to supply free naloxone to anyone at risk of experiencing and/or witnessing an opioid overdose.
For further information or details on how to register your organisation to supply naloxone, including access to mandatory training, please contact naloxone@mhc.wa.gov.au.
Community pharmacies who wish to join the Commonwealth THN Program can register via the online portal.
Opioid Overdose Recognise and Respond Cards are available free to support workers and people who use or know someone who uses opioids.
1. Chrzanowska A, Man N, Sutherland R, Degenhardt L, Peacock A. Trends in overdose and other drug-induced deaths in Australia, 2004-2023. Sydney: National Drug and Alcohol Research Centre, UNSW Sydney; 2025. Available from: https://doi.org/10.26190/unsworks/31245.
Clinicians across Western Australia are invited to join weekly online education sessions about alcohol and other drug (AOD) treatment, hosted by specialist clinicians from the Commission's Next Step Drug and Alcohol Services.
The educational webinars are held every Wednesday at 12:15pm and topics include the assessment of alcohol and other drug issues, managing substance use disorders such as alcohol, opioids, cannabis and methamphetamine, and episodic topics on current AOD issues of interest.
The sessions are held on a ten week rotational basis, however they are continually evolving and often feature guest speakers, so content remains relevant across rotations.
To register contact michael.christmass@health.wa.gov.au.
Next Step Addiction Medicine Symposium, March 2021
Next Step Education Webinars for Clinicians
Contact a specialist Next Step AOD clinician on (08) 6553 0520.
The Mental Health Commission offers a Drug and Alcohol Clinical Advisory Service at no charge to health professionals in Western Australia. The specialist telephone consultancy service is staffed by experienced addiction medicine specialists and provides clinical advice to health professionals on all issues relating to patient management of alcohol and other drug use.
The ASSIST portal has been developed by the University of Adelaide, funded by the Australian Government, to scale up screening and intervention for substance use disorders. It is an electronic version of the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) which was developed by the World Health Organization. The ASSIST has eight questions and takes approximately 5-10 minutes to complete. The ASSIST helps identify the risks associated with substance use and the personalised feedback helps explore options for change. It is for health and welfare professionals to develop knowledge and skills on how to assess and intervene while the ASSISTplus site is to enable self-assessment by people who consume substances. Access it via www.assistportal.com.au
The Drug and Alcohol Counsellors Training Program DVD Resources consists of audio-visual scenarios both with and without teaching text. Expanded text outline key teaching points are also included within this package.
This resource has been designed to support trainers who are delivering training to frontline workers, with the purpose of supporting the workers knowledge, development, competence and confidence of core counselling skills required for effective AOD counselling.
Prior to delivering any training using this package, trainers should familiarise themselves with the audio-visual resource and all information provided in the teaching points. It is highly recommended that presenters are acquainted with relevant core counselling skill literature.
Click here to access a version of these videos without on-screen text.
The Mental Health Commission produces a range of online and physical resources which can be downloaded or ordered from our resources library. Visit the websites below to find and download evidence-based resources that support the community to make informed decisions about alcohol, other drugs, and mental health and wellbeing on mental health, alcohol and other drug topics.
The Commonwealth Department of Health has produced the National Framework for Alcohol, Tobacco and Other Drug Treatment 2019-2029 and the National Quality Framework for Drug and Alcohol Treatment Services.
MHPOD is an evidence-based online learning resource for people working in mental health. Currently, there are over 100 hours of material across 68 topics, written and produced in Australia. The topics range from recovery to legislation and dual disability. The content of MHPOD is linked to the National Practice Standards for the Mental Health Workforce.
Access the MHPOD Learning Portal
The Commission produces a range of resources, checklists, handbooks and information sheets about the Mental Health Act and its application.
Access Mental Health Act resources
The Department of Health has produced a Mental Heath Patient Transport Buyers Guide, which outlines the contract with Wilson Medic One to provide a road-based transport service, in the metropolitan area, for eligible mental health patients who are subject to a transport order or apprehension and return order under the Mental Health Act 2014. In country areas, the existing arrangements with St John Ambulance are to be used.
For clinical mental health resources please visit the Chief Psychiatrist's website or the Department of Health's Mental Health Policy Framework.
Page last updated8 September 2025